Share your perspective and help improve the health of our community! Valley Medical Center is conducting a Community Health Needs Assessment (CHNA), a comprehensive report to help us better understand the health needs of the community our health system serves. Learn more and take the short survey.
Rheumatology & Arthritis

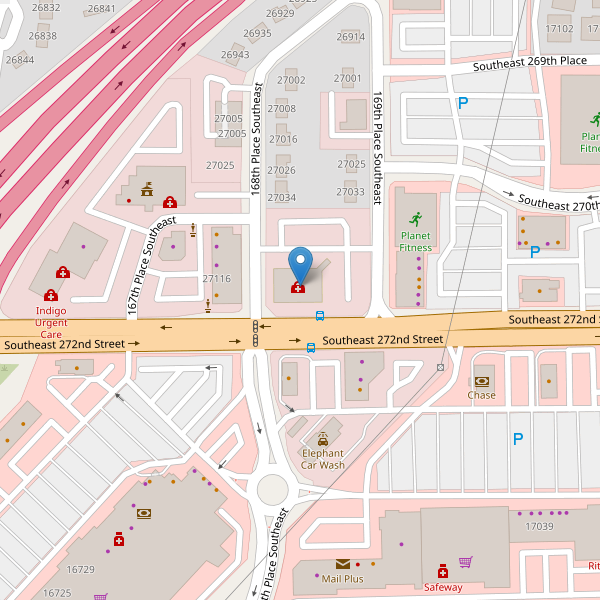
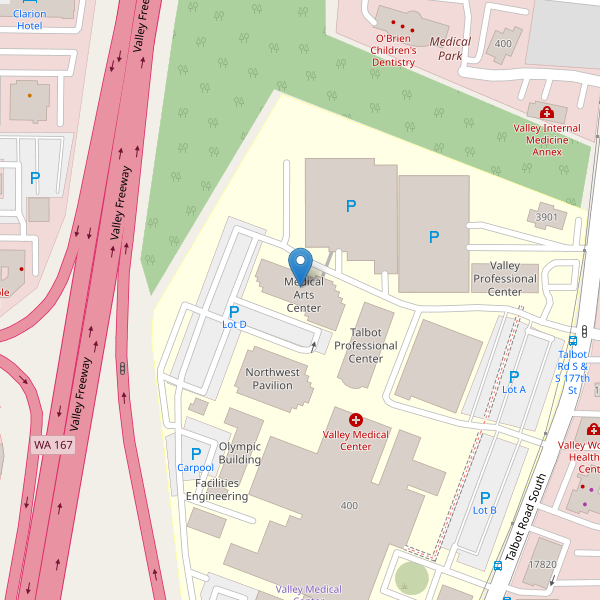
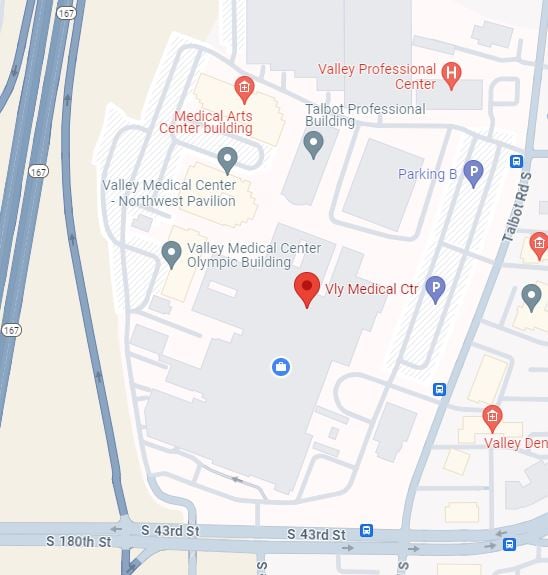
Rheumatology Clinic providers have additional training and experience in the diagnosis and treatment of arthritis and other diseases of the joints, muscles and bones. Valley’s rheumatology providers offer advanced medical treatments including injections with and without guided ultrasound, oral medications, as well as infusion services.
What inflammatory conditions do Valley’s Rheumatology clinic providers diagnose, treat and help manage?
Valley’s Rheumatology Clinic providers specialize in inflammatory arthritis and other autoimmune disorders including: rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, lupus, scleroderma, myositis, Sjogren's syndrome, polymyalgia rheumatica, vasculitis, osteoporosis, tendinopathy, bursitis and gout.
Arthritis is a general term for conditions that affect the joints and surrounding tissues. Joints are places in the body where bones come together, such as the knees, wrists, fingers, toes and hips.The two most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis (OA) is a painful, degenerative joint disease that often involves the hips, knees, neck, lower back or small joints of the hands. OA usually develops in joints that are injured by repeated overuse from performing a particular task or playing a favorite sport or from carrying around excess body weight. Eventually this injury or repeated impact thins or wears away the cartilage that cushions the ends of the bones in the joint. As a result, the bones rub together, causing a grating sensation. Joint flexibility is reduced, bony spurs develop and the joint swells. Usually, the first symptom of OA is pain that worsens following exercise or immobility. Treatment usually includes analgesics, topical creams or nonsteroidal anti-inflammatory drugs (known as NSAIDs); appropriate exercises or physical therapy; joint splinting; or joint replacement surgery for seriously damaged larger joints, such as the knee or hip.
Rheumatoid arthritis (RA) is an autoimmune inflammatory disease that usually involves various joints in the fingers, thumbs, wrists, elbows, shoulders, knees, feet and ankles. An autoimmune disease is one in which the body releases enzymes that attack its own healthy tissues. In RA, these enzymes destroy the linings of joints. This causes pain, swelling, stiffness, malformation and reduced movement and function. People with RA also may have systemic symptoms, such as fatigue, fever, weight loss, eye inflammation, anemia, subcutaneous nodules (bumps under the skin) or pleurisy (a lung inflammation).
Although osteoporosis and osteoarthritis are two very different medical conditions with little in common, the similarity of their names causes great confusion. These conditions develop differently, have different symptoms, are diagnosed differently and are treated differently.
Osteoporosis is a condition in which the bones become less dense and more likely to fracture. It can result in a loss of height, severe back pain and change in one’s posture. Osteoporosis can impair a person’s ability to walk and can cause prolonged or permanent disability.
Studies show that people with OA are less likely than average to develop osteoporosis. On the other hand, people with RA may be more likely to develop osteoporosis. This is especially true because some medications used to treat RA can contribute to osteoporosis. Learn more about osteoporosis.
Osteoporosis and arthritis do share many coping strategies. With either or both of these conditions, many people benefit from exercise programs that may include physical therapy and rehabilitation. In general, exercises that emphasize stretching, strengthening, posture and range of motion are appropriate. Examples include low-impact aerobics, swimming, tai chi and low-stress yoga. However, people with osteoporosis must take care to avoid activities that include bending forward from the waist, twisting the spine or lifting heavy weights. People with arthritis must compensate for limited movement in affected joints. Always check with your doctor to determine whether a certain exercise or exercise program is safe for your specific medical situation.
Most people with arthritis will use pain management strategies at some time. This is not always true for people with osteoporosis. Usually, people with osteoporosis need pain relief when they are recovering from a fracture. In cases of severe osteoporosis with multiple spine fractures, pain control also may become part of daily life. Regardless of the cause, pain management strategies are similar for people with osteoporosis, OA, and RA.
If you have any of the following:
- Swelling in a joint lasting two weeks or longer or new onset of swelling in multiple joints, without fever or signs of infection
- Back pain for longer than one – two months, if you are under age 40 and it’s not related to injury
- Evaluation of osteoporosis or Raynaud’s
- Repeated episodes of uveitis or plantar fasciitis
- Previous diagnosis of rheumatic diseases and transferring care from another rheumatologist
- Gout
*Please consult your primary care provider if you are unsure about your condition and symptoms, or if your insurance requires a referral for specialty care.