Share your perspective and help improve the health of our community! We are conducting a Community Health Needs Assessment (CHNA) to help us better understand the health needs of the community our health system serves. Learn more and take the short survey.
Sleep Medicine & Pulmonary Care

Sleep Medicine
Do you consistently wake up too early or have difficulty awakening? Does your snoring awaken you or your partner? Do you or your partner notice you wake up choking or gasping for breath? These and many other symptoms indicate that you may have a sleep-related problem or a sleep disorder. Studies show 60 percent of American adults experience a sleep problem a few nights a week or more. You may not even be aware of how tired you are, thinking that there is nothing wrong. The great news is most sleep-related problems and sleep disorders can be successfully treated.
Restful sleep is integral to lifetime health. The Sleep Center at Valley is dedicated to the treatment of sleep disorders and sleep-related problems in adults and children.
What are Sleep Studies?
Sleep studies are tests that monitor what happens to your body during sleep. Sleep disorder specialists conduct sleep studies to find out what is causing your sleep problems.
Sleep studies can also determine whether you have a problem with your stages of sleep. The two stages of sleep are non-rapid eye movement (NREM) and rapid eye movement (REM). Normally, NREM and REM alternate four to five times during a night's sleep. A change in this cycle may make it hard for you to sleep soundly.
What is The Sleep Center?
The Sleep Center at Valley Medical Center is a special medical facility designed to evaluate and treat both adults and children with sleep disorders and sleep-related problems. Yet the interior appointments and private, cozy décor of each room feels like a home away from home: patchwork quilts, a private bathroom and shower, and an LCD TV and DVD player. And, of course, a Playstation® 3 for our youngest guests.
The Sleep Center is fully accredited by the American Academy of Sleep Medicine, which means it meets the most rigorous of standards to rank as a center of excellence in the comprehensive management of sleep disorders. Members of our staff are specially trained to study and evaluate people's sleep patterns. The results of our diagnostic studies are used to diagnose and treat sleep problems.
 Why go to The Sleep Center?
Why go to The Sleep Center?
In the past, many sleep disorders were considered untreatable or consequences of normal aging. Today, many disorders can be diagnosed efficiently and treated successfully. There is heightened clinical interest and research in sleep medicine. Much of this excitement stems from our increasing abilities to quickly and successfully help people with their sleep difficulties. Getting a good night's sleep can make a huge difference in a person's life, and The Sleep Center at Valley Medical Center can help achieve this.
There are about 85 recognized sleep disorders, most of which are treatable. A sleep disorder disrupts and disturbs your overall quality of life. More than 70 million people in this country have a sleep disorder.
Many people who have sleep disorders may be completely unaware of it. Perhaps you think you just are sleeping too much or too little, or are tired due to jet lag. Some sleep behavior may be only noticeable by your bed partner, such as moving your arms or legs, talking, or sleepwalking. Or maybe you wake up with a sore jaw and don't know why.
Visit our health library to learn more about some of the most common disorders:
Heart Disease & Sleep Disorders: Untreated, obstructive sleep apnea is associated with an increased risk of high blood pressure, heart attack, irregular heartbeats, heart failure and stroke. Treatment can help improve breathing and reduce the severity of symptoms such as loud snoring and excessive daytime sleepiness, thereby improving sleep-related quality of life and performance at work or in school.
The American Academy of Sleep Medicine recommends these guidelines for good sleeping habits, which can be used for all types of sleep disorders:
 Get up about the same time every day.
Get up about the same time every day.- Go to bed only when sleepy. Establish relaxing presleep rituals, such as a warm bath, light bedtime snack, or 10 minutes of reading.
- Exercise regularly. Confine vigorous exercise to early hours of the day. Mild exercise should occur at least 4 hours before bedtime.
- Keep a regular schedule. Normal times for meals, medications, and activities help keep our inner clocks running smoothly.
- Avoid caffeine within 6 hours of bedtime.
- Do not drink alcohol, especially when sleepy.
Do You have a sleep disorder?
Sleep disorders come in many forms. The problem may be obvious; you may fall asleep constantly at meetings or your bed partner may wake you because of irregular breathing patterns. Symptoms may be more subtle or even unnoticeable; you may experience long-term fatigue or general irritability.
Some people realize they have a sleep disorder because of specific symptoms, such as remembering waking up frequently. Others may have a sleep disturbance without realizing it at all, with sleep disruption occurring too briefly to be remembered. A primary symptom is daytime sleepiness, which may be perceived as normal, despite the concerns of friends, family and coworkers.
Anyone persistently exhibiting the following symptoms or conditions should consider getting evaluated by a physician specially trained in sleep medicine:
- Irregular breathing during sleep; excessive sleepiness during the day.
- Falling asleep at inappropriate times (while driving, during meetings, etc.)
- Temporary weakness of body or speech muscles occurring with excitement, anger or other strong emotions; sleep walking or talking.
- Experiencing nightmares or disturbing dreams.
- Having sleep-related seizures; difficulty with working nights or rotating shifts
- Repeated movements or twitching of the legs or arms during sleep (may be noticed only by bed partner)
- Dissatisfaction with the amount or quality of sleep.
- Difficulty with winter-time sleepiness or depression (Seasonal Affective Disorder, or SAD).
Learn more about sleep evaluation and testing.
Patient Education and Support Groups
Valley Medical Center offers classes in a variety of areas affecting your health and well-being that may also affect your sleep health, such as weight management, fitness, and cardiac health.
Sleep Web Sites
American Academy of Sleep Medicine
National Sleep Foundation
National Heart, Lung, and Blood Institute
American Sleep Apnea Association
Restless Legs Syndrome Foundation
Narcolepsy Network
Academy of Dental Sleep Medicine (ADSM)
American Association of Sleep Technologists
Journal SLEEP
Pulmonary Care
Valley Medical Center's Pulmonary Services specializes in the diagnosis and treatment of problems related to the lungs and airway like asthma, emphysema, sleep disorders, interstitial lung diseases and pneumonia. In addition, we provide comprehensive care for lung cancer patients and individuals with pulmonary vascular disease.
Check out our articles for patients, families and caregivers:
Learn how to live well with asthma or chronic lung disease (COPD).
What is a pulmonologist?
A pulmonologist is specially trained in diseases and conditions of the chest, such as pneumonia, asthma, tuberculosis, emphysema or complicated chest infections.
When do you need a pulmonologist?
Not everyone who suffers from an acute respiratory condition or chronic respiratory disease needs a pulmonologist. Many of these conditions can be managed by a general internist. Their skills are usually needed for patients with complex pulmonary problems, such as emphysema, tuberculosis, asthma, complicated infections of the chest, the pulmonary complications of AIDS, injury and complications of respiratory diagnostic and therapeutic procedures.
Does a pulmonologist perform surgery?
Major surgical procedures are performed by a thoracic surgeon. Yet pulmonologists often perform specialized procedures to obtain samples of the lining of the chest wall or of the lung itself. For example, they use flexible fiberoptics to see inside the air passages and extract sample pieces for study.
An Individualized, Supervised Program Just for You
 Valley's Pulmonary Rehabilitation program specializes in the diagnosis and treatment of problems related to the lungs and airway like chronic obstructive pulmonary disease (COPD), emphysema, and pulmonary hypertension and fibrosis. In addition, comprehensive care is available for patients with lung cancer and in association with lung cancer surgery.
Valley's Pulmonary Rehabilitation program specializes in the diagnosis and treatment of problems related to the lungs and airway like chronic obstructive pulmonary disease (COPD), emphysema, and pulmonary hypertension and fibrosis. In addition, comprehensive care is available for patients with lung cancer and in association with lung cancer surgery.
Helping you breath easier.
Providers at Pulmonary Rehab treat patients with lung problems such as: Chronic Obstructive Pulmonary Disease (COPD), chronic bronchitis, emphysema, bronchiectasis, sarcoidosis, pulmonary hypertension, idiopathic pulmonary fibrosis, interstitial lung disease, lung cancer and lung cancer surgery, and lung volume reduction surgery before and after lung transplant
Pulmonary Rehabilitation includes exercise classes and education about your lung disease or condition. PR may help you participate in activities with less shortness of breath, as well as teach you how to live better by managing your lung condition.
What are the benefits of Pulmonary Rehabilitation?
Pulmonary rehabilitation helps you improve the quality of your life. Although PR can't cure your lung disease, it can make breathing easier and allow you to experience fewer problems.
Other benefits include a decrease in the symptoms of your disease or condition; an improvement in your ability to function better in daily life; an increase in your ability to exercise; reduced symptoms of dyspnea and leg pain; a decrease in your symptoms of anxiety and depression and improvement in your ability to manage them; the ability to make the most of the lung function you have; an increase in your overall stamina and energy; reduced hospitalization / unscheduled healthcare visits
What's Included in the Program?
 Monitored & Supervised Exercise
Monitored & Supervised Exercise
A primary focus of pulmonary rehab is to improve your cardiorespiratory function through exercise. This is achieved by strategic implementation of cardiovascular, strength, flexibility, and breathing training protocols. This physician-led program allows patients to exercise in a safe environment under the watchful eyes of respiratory and exercise therapists. Your program will be individualized to meet you at any level.
Education Programs
Valley's education classes focus on COPD, as well as other chronic lung diseases, providing information on medications, their actions, aside effects, using an inhaler and self-care techniques; understanding and using oxygen therapy; retraining breathing; importance of exercise; strategies for managing breathing problems; symptom assessment and knowledge about when to seek medical treatment; reducing and controlling breathing difficulties and other symptoms; earning more about your disease, treatment options and chronic disease coping strategies; learning to manage your disease and reducing your dependence on costly medical resources; maintaining healthy behaviors such as smoking cessation, good nutrition and weight management.
Emotional Support
People who have chronic lung diseases are more prone to depression, anxiety and other emotional problems. By participating in Valley Medical Center's Pulmonary Rehabilitation program, you will have the support and resources to help you along your healthy lifestyle journey.
Other Services
A big part of learning how to best improve your symptoms is learning about your bodies specific nutritional needs. Consult with one of our registered dieticians to identify a healthy nutrition plan.
If you have been dealing with chronic aches and pains, meet with a physical therapist to help identify what will be the best approach to reaching your fitness goals.
 Click here to download a pdf of the information to take to your physician.
Click here to download a pdf of the information to take to your physician.
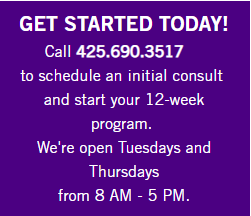
GET STARTED TODAY!
Call 425.690.3517 to schedule a consult and start your 12-week program.