Share your perspective and help improve the health of our community! Valley Medical Center is conducting a Community Health Needs Assessment (CHNA), a comprehensive report to help us better understand the health needs of the community our health system serves. Learn more and take the short survey.
Diabetes & Thyroid (Endocrinology)

We empower you to live a healthy life
Valley takes a comprehensive, team approach to managing diabetes and thyroid disorders. Our endocrinologists partner with patients and their primary care providers to help patients take charge of their health and achieve a better quality of life. It is our goal to halt or slow progression of disease through treatment, education and lifestyle optimization. We also offer diabetes education, which is covered by many insurance plans. Our diabetes educators and dietitians can help you learn how to live well with diabetes - learn more here!
An endocrinologist is a specially trained doctor who can diagnose diseases that affect your glands. They know how to treat conditions that are often complex and involve many systems within your body. Your primary-care physician refers you to an endocrinologist when you have a problem with your endocrine system.
The endocrine system is a complex group of glands. Glands are organs that make hormones. These are substances that help to control activities in your body. Different types of hormones control reproduction, metabolism (food burning and waste elimination) and growth and development. Hormones also control the way you respond to your surroundings, and they help to provide the proper amount of energy and nutrition your body needs to function. The glands that make up the endocrine system include the thyroid, parathyroid, pancreas, ovaries, testes, adrenal, pituitary and hypothalamus.
Endocrinologists are trained to diagnose and treat hormone imbalances and problems by helping to restore the normal balance of hormones in your system. They take care of many conditions, including:
- Diabetes
- Thyroid disorders
- Metabolic disorders
- Adrenal disorders
- Over- or under-production of hormones
- Menopause
- Osteoporosis
- Hypertension (high blood pressure)
- Cholesterol (lipid) disorders
- Lack of growth (short stature)
- Cancers of the endocrine glands
Endocrinologists also conduct basic research to learn the way glands work and clinical research to learn the best methods to treat patients with a hormone imbalance. Through research, endocrinologists develop new drugs and treatments for hormone problems.
Diabetes Education & Nutrition
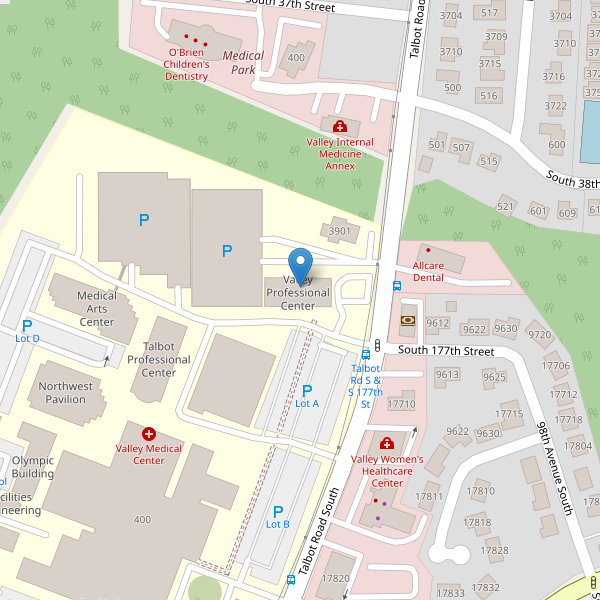
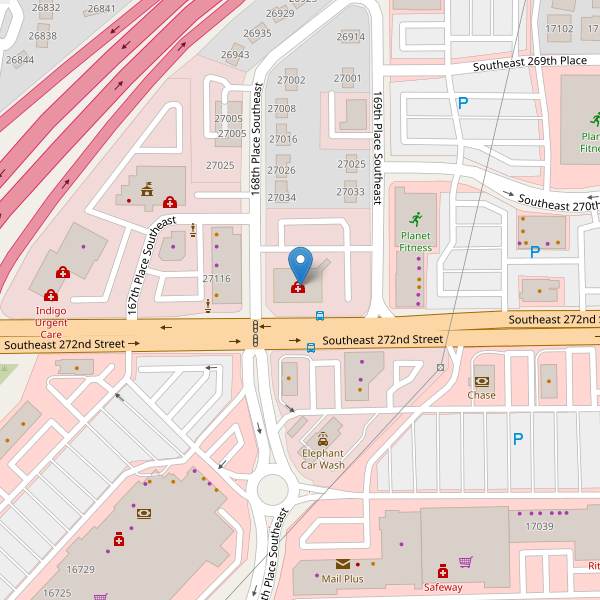
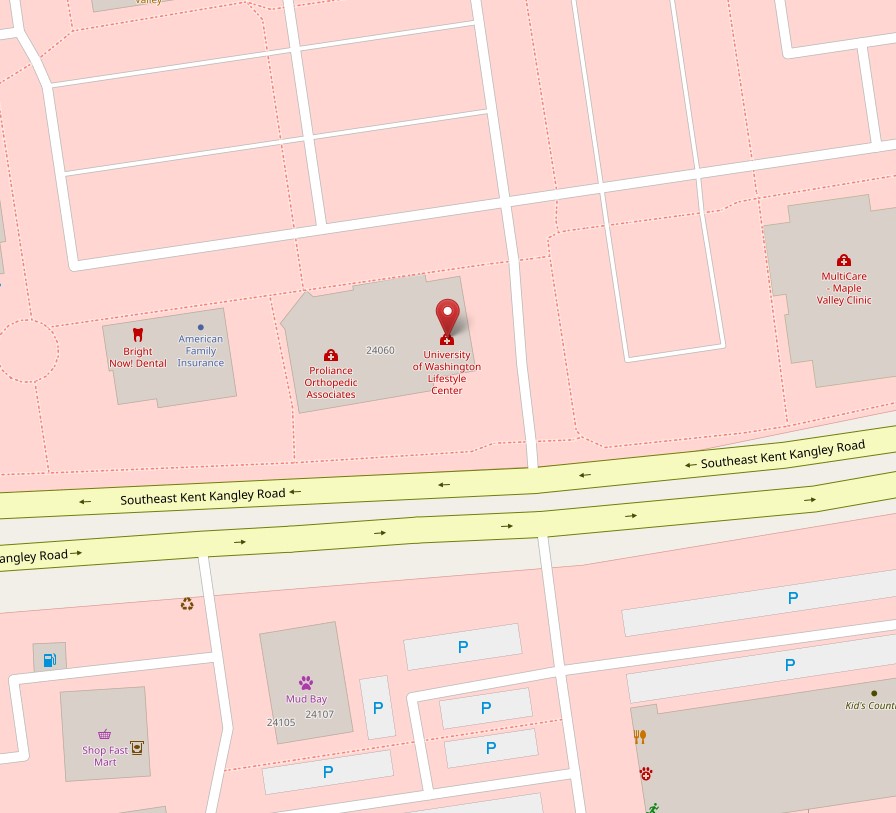
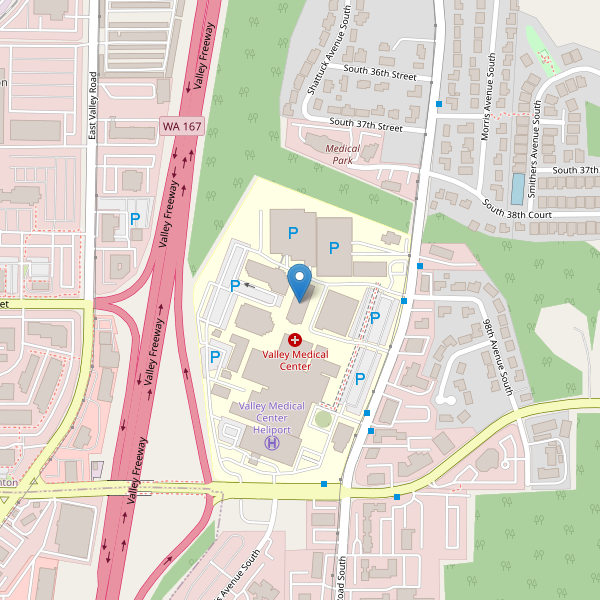
Valley provides nutritionists and Certified Diabetes Education & Care Specialists (CDCES) at several Lifestyle Medicine locations, including Renton, Covington and Maple Valley. We provide a full complement of education and services focused on prevention and management to halt or slow progression of disease. We serve those who are pre-diabetic, have gestational diabetes and those with Type 1 and Type 2 diabetes.
Diabetes is a complex disease that requires daily self-management, making healthy food choices, staying physically active, monitoring your blood sugar and taking medications as prescribed. It is also important to talk regularly with your diabetes care team to problem solve, reduce risks for complications and cope with lifestyle changes.
Successful self-management will help you feel better and can reduce your chance of developing complications including heart disease, dental disease, eye disorders, kidney disease, nerve damage and lower leg amputation.
Diabetes management can feel overwhelming at times as you manage food, physical activity, blood sugar monitoring and medications at the same time. It is not uncommon to experience fear, anger, or stress. Our team of Registered Dietitians and Diabetes Educators can partner with you and help you navigate barriers along the way.
The program is designed to help you learn how to take care of yourself, guide you through your treatment and help you with any fears, issues and problems you encounter along the way.
Our diabetes program consists of three weekly group education classes available in-person or online. After completing the class series, individuals are scheduled for a 1:1 visit with the registered dietitian to personalize their nutrition and lifestyle goals. We also provide ongoing support through our monthly diabetes support group.
What is diabetes?
Diabetes is a metabolic disorder where the pancreas produces little or no insulin, causing blood sugar to rise.
What are the symptoms of diabetes?
The most common symptoms are frequent urination, blurred vision, wounds that don’t heal, frequent infections, increased thirst and chronic fatigue. If you have these symptoms or a family history of diabetes, see your doctor for a blood test.
What is the difference between Type 1 and Type 2 diabetes?
Type 1 diabetes (about 10 percent of people with diabetes) is an autoimmune disease in which the immune system attacks the cells of the pancreas that produce insulin. Type 2 diabetes (about 80 to 90 percent of persons with diabetes) is a progressive chronic disease that affects insulin production and utilization. Generally, individuals who have Type 2 diabetes still produce insulin, though not as efficiently.
What is the treatment for diabetes?
Medical treatment centers on controlling blood sugar as well as preventing and monitoring for complications. Teaching people how to manage their diabetes and regular follow-up with their healthcare provider is essential for long-term wellness. People learn to monitor their blood sugar and are treated medically for blood sugar control. Persons with Type 1 diabetes require insulin injections for blood sugar control and ultimately for their survival. Persons with Type 2 diabetes may be able to control blood sugar by making lifestyle changes and/or through oral medications. Insulin may be required depending on the person’s ability to manage their blood sugar by other means.
Is it true that only kids get Type 1 diabetes and only adults get Type 2 diabetes?
Commonly Type 1 diabetes manifests in childhood and teenage years, though it can occur at anytime of the life cycle. Type 2 diabetes previously was called adult-onset diabetes. We are now seeing Type 2 manifesting at all ages, even in children.
What are the medical complications associated with diabetes, and how do providers monitor these complications?
Complications associated with diabetes include increased risk for heart disease and stroke, damage to small blood vessels of the eyes and kidneys, and damage to the nervous system. Persons with diabetes should see their healthcare provider regularly, every 3 to 6 months. Patients are monitored for blood sugar and blood pressure control and evaluated and/or treated for underlying cardiovascular disease. Exams or tests done annually include dilated eye exam, foot exam, blood cholesterol, and urinalysis to monitor for kidney changes.
How do healthcare providers monitor blood sugar control?
A blood test called the hemoglobin A1c is used to determine blood sugar control. This test measures the percentage of hemoglobin (a blood protein) that has sugar or glucose attached. The higher the percentage, the higher the blood sugar has been over the previous 2 to 3 months. The results more closely reflect blood sugar levels occurring within the month prior to the blood draw.
How can individuals with diabetes decrease their risk of developing the complications associated with diabetes?
Following a healthy lifestyle will decrease the risk of heart disease and stroke. Blood sugar and blood pressure control play an important role in significantly reducing the risk of complications. One of the most important things individuals with diabetes can do is to become educated about managing their diabetes. Lifestyle Medicine at Valley Medical Center offers classes that empower individuals to make lifestyle choices that will promote their health and well-being.
Will insurance cover diabetes education classes?
Typically most insurance companies cover diabetes education to some extent if the deductible has been met. We recommend that you check with your insurance company to verify coverage of diabetes education classes.
How can I get a test for diabetes?
See your family medicine doctor, who will test your fasting blood sugar or random blood sugar levels.
In addition to medication, how can I lower my blood sugar levels?
In addition to taking medication, you can lower blood sugar levels by educating yourself, making healthy food choices, increasing activity levels, and decreasing stress levels.
What Is a Diabetes Care and Education Specialist?
What We Offer
- Certified Diabetes Education & Care Specialists (CDCES)
- Registered Dietitians (RD)
- Diabetes education workshops
- Gestational diabetes education
- Take home resources and materials
- Individual appointments with regular follow-ups
- Recommendations to community resources
- Access to consultations with exercise specialists and physical therapists
- Understand how your medications work and how to manage them safely